Internal Pelvic Floor Physical Therapy Explained.
Authored by Dr. Maryssa Steffen, PT, DPT, Board-Certified Pelvic Health Specialist
Pelvic Therapy and Internal Pelvic Floor Therapy
A trauma-informed, somatic approach
Pelvic therapy and internal pelvic floor therapy are modalities used by trained, board-licensed physical therapists to assess and treat pelvic floor dysfunction. Each therapist at Bodyful Physical Therapy has over 5,000 hours of experience treating pelvic floor dysfunction across the lifespan and across genders, using both internal and external pelvic floor therapy techniques.
This work is grounded in trauma-informed care, consent, and a somatic approach to healing.
What Is Internal Pelvic Floor Therapy?
Internal pelvic floor therapy can be part of a comprehensive pelvic physical therapy assessment designed to understand the root contributors to your symptoms.
“Internal” refers to consensual intra-vaginal or intra-rectal touch performed by a pelvic therapist using a gloved, lubricated finger to penetrate vaginally or rectally. This approach is slow, collaborative, and therapeutic—not pathologizing or rushed.
You may always choose to begin with gentler, slower, or fully external approaches. Internal work is never required.
You can learn more about starting slowly and building safety here.
Internal assessment is typically offered after evaluating breathing patterns, posture, the diaphragm, abdomen, hips, and spine—because the pelvic floor does not function in isolation.
A Somatic and Trauma-Informed Approach to Pelvic Floor Therapy
The pelvic floor is integrated with breath, posture, and the nervous system. When you begin to sense your breath and core support in ways that shift your symptoms and body awareness, internal pelvic floor work often becomes more accessible to learning about your body.
When you are oriented to your breath and grounded in your body, your pelvic floor muscles may feel easier to sense and explore. This is often where symptom change begins—not through urgency, but through awareness and curiousity.
With informed consent, your therapist may offer internal pelvic floor therapy. At Bodyful, we attend to comfort, communication, temperature, positioning, pacing, and emotional cues throughout this work. Grounding resources and check-ins are built into every session so that the duration, pressure, and type of touch remain supportive.
Why Assess the Pelvic Floor Muscles?
If pelvic symptoms are limiting your movement, function, or quality of life, assessing the pelvic floor muscles may be helpful.
A healthy muscle group:
Is not overly sensitive to touch
Can contract and relax voluntarily
Coordinates with breath and movement
Has flexibility, endurance, and strength
Pelvic physical therapists are uniquely trained to evaluate movement dysfunction, coordination patterns, and anatomical contributors to symptoms—and to guide you toward sustainable, embodied solutions.
During an internal pelvic floor examination, your therapist gently explores the pelvic floor muscles to rule in or rule out contributors to your symptoms. You receive real-time feedback to build body awareness, begin to train coordination for functional movement patterns, and explore the possibilities of expanded movement choices.
What Does “Internal” Mean in Pelvic Therapy?
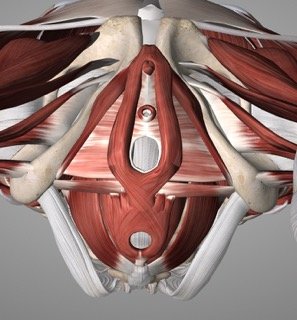
The pelvic floor consists of layered muscles surrounding the pelvic organs and sphincters. To assess and treat these tissues, pelvic therapists use gentle manual techniques and tactile and verbal feedback to support coordination, relaxation, strength, and symptom relief.
Internal means that your pelvic floor therapist uses embodied touch to assess the performance of your pelvic floor muscles by vaginal or rectal penetration with a single, gloved lubricated finger.
If you are not comfortable with your therapist performing the intra-vaginal/rectal assessment, your therapist can definitely teach you how to do it yourself in-person or virtually.
You may also hear about biofeedback, which can include:
Surface EMG sensors with visual feedback
Real-time tactile and verbal cueing from your therapist
Mirror feedback or guided self-touch
Many people benefit most from skilled hands-on assessment paired with somatic cueing rather than devices alone.
Pelvic floor muscles, front view, with the psoas and inner thigh muscles.
Superficial pelvic floor muscles with the pubic bone and tailbone.
What to Expect During a Pelvic Therapy Evaluation
A pelvic therapy evaluation includes far more than the pelvic floor.
Your assessment may involve:
Lumbosacral spine and sacroiliac joints
Abdomen, diaphragm, iliopsoas, piriformis, hips
Abdominal viscera and bladder sensitivity
Screening for diastasis recti or hernias
Posture, breathing, balance, and movement patterns important for daily activities
After some of the above orthopedic assessments, the pelvic floor assessment may be recommended. You would be undressed from the waist down and your external pelvic floor tissues may be observed for scars, irritation, hemorrhoids, pelvic organ prolapse, or hormonal tissue changes. Breath coordination, endurance holds, relaxation, and isolation cues are introduced gradually.
When internal work is appropriate, consensual, and there is enough time, your therapist will move forward with embodied touch with penetration. Your therapist will question your pelvic floor coordination with breath, strength, endurance, flexibility, relaxation after contraction, and symmetry. Gentle manual therapy may be used to decrease tenderness or reproduce and resolve symptoms.
Benefits of Pelvic Floor Therapy
Many people are told to “just do Kegels” without guidance on breathing, coordination, or relaxation. For some, this worsens symptoms.
Pelvic floor dysfunction often involves timing, coordination, and the ability to fully relax, not just gripping. A somatic pelvic therapy approach helps you learn how your body responds—and how to work with it rather than against it.
Conditions Treated with Pelvic Therapy
Pelvic floor physical therapy can support:
Urinary incontinence (leakage with coughing, running, lifting, laughing)
Urinary urgency and overactive bladder
Pelvic organ prolapse (including non-surgical management)
Pain with sex (burning, sharp pain, pain with arousal or orgasm)
Bladder pain without infection
Constipation, IBS, bloating, rectal pain
Pelvic, tailbone, hip, and nerve pain (including sciatica and pudendal symptoms)
Prenatal and postpartum pelvic therapy
Perimenopause and postmenopause care
Care for all genders, including cis, trans, and non-binary bodies
Pelvic Floor Therapy Techniques
Treatment may include:
Pelvic floor relaxation with breath and positioning
Pelvic floor strengthening integrated with posture and movement training
Manual therapy for muscles, fascia, and scar tissue
Coordination training for functional activities
Somatic education and home practices
Surface EMG biofeedback may be helpful for some, though research shows skilled pelvic therapy alone is often equally effective.
Frequently Asked Questions
Can pelvic floor therapy work without internal treatment?
Yes. Many people experience meaningful changes through external work, breathing, posture training, abdominal and diaphragm treatments, and movement retraining alone.
Is internal therapy okay during menstruation?
Yes, if you are comfortable enough to travel.
Do you treat men and trans folks?
Yes. Pelvic floor therapy is gender-inclusive and considers posture, breath, mobility, and coordination across bodies.
Pelvic Therapy in Oakland, CA
If you are seeking trauma-informed pelvic therapy, somatic pelvic floor therapy, or comprehensive pelvic physical therapy, we are here to support you.